Patients who take psilocybin for treatment-resistant depression show reduced symptoms weeks after treatment following a “reset” of their brain activity, according to new research.
For the study, researchers at Imperial College London used psilocybin, the psychoactive compound that occurs naturally in “magic mushrooms,” to treat a small number of patients with depression in whom conventional treatment had failed.
In the study, published in the journal Scientific Reports, researchers describe patient-reported benefits lasting up to five weeks after treatment.
They theorize that the psychedelic compound may effectively reset the activity of key brain circuits known to play a role in depression.
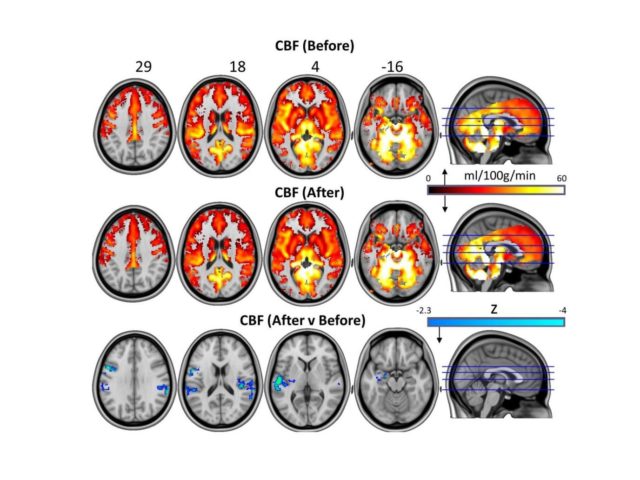
A comparison of images of patients’ brains before and one day after they received the drug treatment revealed changes in brain activity that were associated with marked and lasting reductions in depressive symptoms, according to the researchers.
“We have shown for the first time clear changes in brain activity in depressed people treated with psilocybin after failing to respond to conventional treatments,” said Dr. Robin Carhart-Harris, head of Psychedelic Research at Imperial, who led the study.
“Several of our patients described feeling ‘reset’ after the treatment and often used computer analogies. For example, one said he felt like his brain had been ‘defragged’ like a computer hard drive, and another said he felt ‘rebooted.’
“Psilocybin may be giving these individuals the temporary ‘kick start’ they need to break out of their depressive states and these imaging results do tentatively support a ‘reset’ analogy. Similar brain effects to these have been seen with electroconvulsive therapy.”
For the study, which researchers say is the first with psilocybin in depression, 20 patients with a treatment-resistant form of the disorder were given two doses of psilocybin (10 mg and 25 mg), with the second dose a week after the first.
Nineteen of the patients underwent initial brain imaging and then a second scan one day after the high dose treatment.
The researchers used two main brain imaging methods to measure changes in blood flow and the crosstalk between brain regions, with patients reporting their depressive symptoms through completing clinical questionnaires.
Immediately following treatment with psilocybin, patients reported a decrease in depressive symptoms, corresponding with anecdotal reports of an “afterglow” effect characterized by improvements in mood and stress relief, the researchers report.
Functional MRI imaging revealed reduced blood flow in areas of the brain, including the amygdala, a small, almond-shaped region of the brain known to be involved in processing emotional responses, stress and fear. They also found increased stability in another brain network, previously linked to psilocybin’s immediate effects as well as to depression itself.

These findings provide a new window into what happens in the brains of people after they have “come down” from a psychedelic, where an initial disintegration of brain networks during the drug trip is followed by a re-integration afterwards.
“Through collecting these imaging data we have been able to provide a window into the after effects of psilocybin treatment in the brains of patients with chronic depression,” Carhart-Harris explained.
“Based on what we know from various brain imaging studies with psychedelics, as well as taking heed of what people say about their experiences, it may be that psychedelics do indeed ‘reset’ the brain networks associated with depression, effectively enabling them to be lifted from the depressed state.”
The researchers note that while the initial results of the experimental therapy are exciting, they are limited by the small sample size, as well as the absence of a control group to directly contrast with the patients.
They also note that the research is at an early stage and that patients with depression should not attempt to self-medicate, as the team provided a special therapeutic context for the drug experience and things may go awry if the extensive psychological component of the treatment is neglected.
The researchers plan to test psilocybin against a leading antidepressant in a trial set to start early next year.
“Larger studies are needed to see if this positive effect can be reproduced in more patients. But these initial findings are exciting and provide another treatment avenue to explore,” said Professor David Nutt, a professor of neuropsychopharmacology and director of the Neuropsychopharmacology Unit in the Division of Brain Sciences, and senior author of the paper.
Source: Imperial College London